Table of Contents
ToggleStarting Your Journey
A vasectomy is a significant decision in one’s life, often taken after thorough deliberation. It’s a permanent form of birth control so understanding the vasectomy process and its implications is crucial before having the procedure.
Why Choose a Vasectomy?
Vasectomies offer a reliable and permanent solution to prevent pregnancy. Compared to tubal ligation in women, vasectomies are less invasive, carry fewer risks and are often more cost-effective. It’s important to consider this option if you are certain about not wanting more children.
Discussing with Your Partner and Doctor
Before undergoing a vasectomy, it’s vital to have open discussions with your partner and seek a doctor’s advice. This ensures that both parties are comfortable with the decision and understand that vasectomy is a permanent form of birth control.
Vasectomy Process: What You Need to Know
Understanding the vasectomy procedure, from its methodology to recovery, helps demystify the vasectomy process.
The MSI No-Scalpel Open-Ended Technique
A vasectomy is a minor surgical procedure that involves blocking the vas deferens, the tubes that carry sperm, to prevent sperm cells from mixing with semen. We only use the MSI No-Scalpel Vasectomy technique, which requires only a tiny puncture in the skin, meaning there’s no need for stitches, unlike a conventional vasectomy.
Debunking Common Myths
Common myths, such as vasectomies leading to prostate cancer, testicular cancer, or a decrease in sex drive, are unfounded. Vasectomies do not affect sexual performance and are not linked to these health issues.
Preparing for Your Vasectomy
Preparation for a vasectomy includes consultations and understanding the procedure, which uses IV sedation or local anaesthetic to minimise discomfort.
Pre-Procedure Consultation and Checks
Before the vasectomy, your doctor will conduct a thorough medical check-up to ensure you’re a suitable candidate. This includes discussing your health history and understanding potential risks like post-vasectomy pain syndrome.
What to Do in the Days Leading Up to Surgery
In the days leading up to the surgery, follow your doctor’s instructions, which may include stopping certain medications and arranging for a recovery period. This preparation ensures the procedure goes smoothly.

The Day of the Procedure
Understanding what happens during the procedure can alleviate anxiety and prepare you for a smooth experience:
- Before the procedure begins, you may be asked to change into a medical gown.
- Unfortunately, any accompanying support person will not be allowed to stay with you in the procedure room. They may choose to leave the clinic and return at a later time.
- Before starting, you will receive the anaesthetic you selected. For those opting for IV sedation, it’s crucial to thoroughly read the provided sedation information booklet.
- The doctor will administer a local anaesthetic to numb the scrotum area. Then, they will create a small incision to reach the vas deferens and seal the upper end.
- Typically, this procedure is performed without a scalpel and does not require external stitches.
- After the procedure, a small dressing will be applied to the incision area.
- The entire vasectomy process is generally completed in no more than 15 minutes.
Immediate Post-Procedure Care
After your vasectomy, a smooth and quick recovery (usually less than a week), is within reach if you follow your doctor’s advice. It’s normal to feel a bit uncomfortable right after the procedure, but don’t worry – a little rest, some ice packs for any swelling, and over-the-counter painkillers should help do the trick.
Try to take it easy, especially for the first few days; avoiding too much walking or standing can really help and remember, if you feel any severe pain, let your doctor know right away.
Emotional and Psychological Recovery
The emotional and psychological impact post-vasectomy is as important as the physical recovery. After a vasectomy, it’s normal to experience a range of emotions. Engaging in open communication with your partner can help in adjusting to this change.
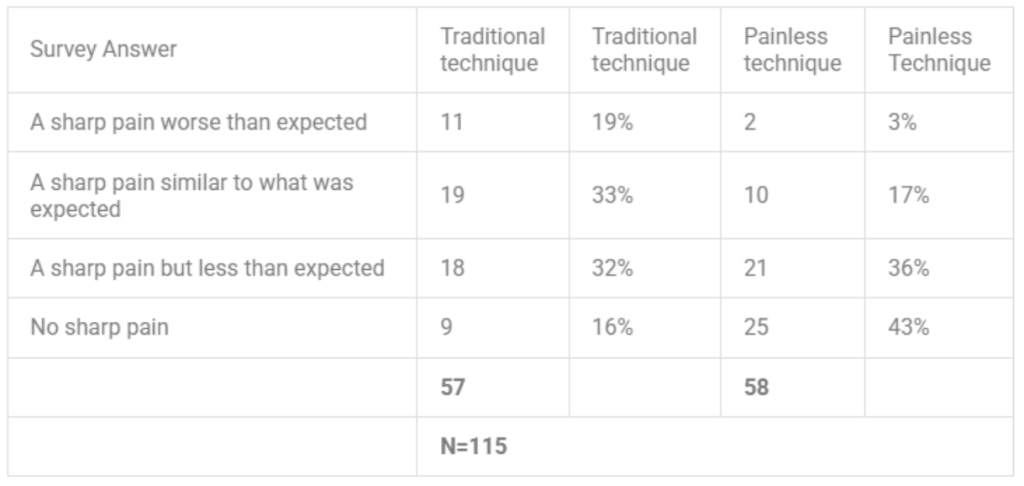
Is it painful to have a vasectomy?
The procedure itself is not painful due to the local anaesthetic, though some men may experience mild pain or discomfort afterwards, which is typically manageable.
Who can have a vasectomy?
Any man who wants a permanent form of birth control can consider a vasectomy. However, it’s important to discuss with a doctor to ensure it’s the right choice, particularly for those with certain medical conditions or concerns about vasectomy reversal in the future.
When can I resume sexual activity?
You should avoid any sexual activity for at least 7 days after having a vasectomy. It’s also important that for the first 3 months after the procedure you use another method of contraception, as it can take this long to clear the remaining sperm. Keep using contraception until a semen test shows a zero sperm count.
Does a vasectomy protect you from getting sexually transmitted infections?
No, a vasectomy does not protect against sexually transmitted infections (STIs). While it is an effective method for preventing pregnancy by stopping the release of sperm, it does not prevent the transmission of STIs. You should still use condoms or other protective measures to guard against STI transmission during sexual intercourse.
Are there any risks associated with having a vasectomy?
Vasectomies are typically low-risk procedures, yet they can lead to short-term discomfort or pain in the immediate aftermath. While instances of chronic pain are exceptionally rare following a vasectomy, there are effective treatments available for those who experience this. It’s reassuring to note that the majority of these cases resolve completely over time, ensuring that long-term complications remain uncommon.