Table of Contents
Don’t worry it’s not a hit to the balls
Most men have, at some point in their lives, experienced an impact or blow to their testicles. It’s an unfortunate side-effect of having them located where they are. For many men, just the recollection of such an event is enough to bring tears to their eyes. And this memory is often one of the factors that deter men from committing to a vasectomy. So is getting a vasectomy as painful? Read on to find out the good news.
The good news
However, the vasectomy procedure itself is actually close to painless. The majority of the time your vasectomist won’t be touching your testicles at all, their attention will be on a small amount of scrotal skin that will be pinched open and through which they will work on your vas deferens.
The reason why it’s virtually painless
The first part of the vasectomy procedure involves the application of a local anaesthetic to your scrotum. This ensures that throughout the procedure you won’t feel anything, except some distant tugging and, at worst, a mild ache.
The application of the local anaesthetic is done via a needle – this might seem daunting, given its destination, however, our National Director of Vasectomy Services, Dr Justin Low, has pioneered a way to make it as painless as possible.
Don’t just take our word for it
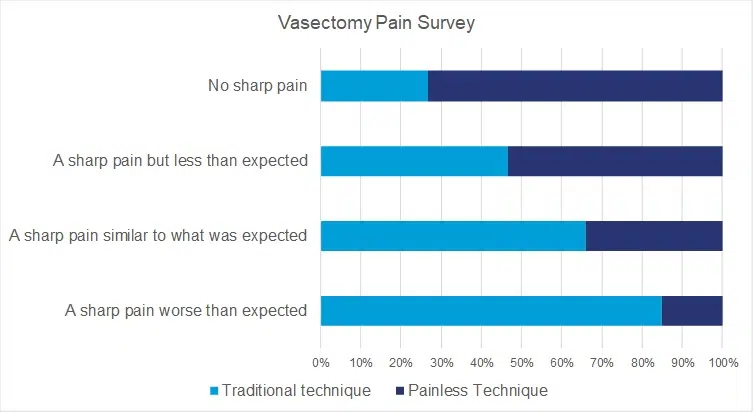
To determine that this was the case, we surveyed a number of men after their procedure to establish how effective the method was across a broad cross-section.
115 vasectomy patients responded to our survey. Half had received their anaesthetic via the new technique, and the other half received it via the traditional technique. The results confirmed what we knew to be a significant advancement in vasectomy techniques.
The Results
Both sets of patients were asked to register one answer (multiple choice) to the same question.
The question was: “During a vasectomy procedure many patients experience some minor aching, pulling and stretching feelings during the procedure.
However, specifically in relation to the needle used to deliver the local anaesthetic, we would like to know if you felt: A) A sharp pain worse than expected B) A sharp pain similar to what was expected C) A sharp pain but less than expected D) No sharp pain.”
We think the results speak for themselves.
| Survey Answer | Traditional technique | Traditional technique | Painless technique | Painless Technique |
| A sharp pain worse than expected | 11 | 19% | 2 | 3% |
| A sharp pain similar to what was expected | 19 | 33% | 10 | 17% |
| A sharp pain but less than expected | 18 | 32% | 21 | 36% |
| No sharp pain | 9 | 16% | 25 | 43% |
| 57 | 58 | |||
| N=115 | ||||
Results may vary. Click here for more on the survey methodology.
19% of men who had the traditional method of anaesthetic delivery reported feeling “a sharp pain, worse than expected.” By contrast, 79% of men who received anaesthetic through Dr Low’s method reported that it was “a sharp pain, but less than expected” (36%) or “no sharp pain” at all (43%).
So if you were holding off on having a vasectomy done because you were worried about the pain of the procedure, that’s one less reason to worry!
How long does the pain last after a vasectomy?
Pain after a vasectomy typically lasts for about 3 days but may vary depending on individual healing and recovery. Some men may experience post-vasectomy pain syndrome, a rare condition characterised by chronic pain in the scrotal area, which may require further medical intervention.
How long does it take to feel normal after a vasectomy?
Most men start to feel normal within a week after the procedure, although complete recovery may take up to two weeks. During this time, it’s important to follow your doctor’s recommendations to avoid complications and manage any discomfort.
Are there any risks or side effects?
Yes, there are potential risks and side effects associated with a vasectomy. While generally considered a safe procedure, some possible complications include infection, as with any surgical procedure, and bleeding or blood clot formation in the scrotum. In rare cases, some men may experience chronic scrotal pain or post-vasectomy pain syndrome.
What can I expect during and after having a vasectomy?
During a vasectomy, the vas deferens, which carry sperm, are cut, sealed, or blocked to prevent sperm from mixing with semen. You can expect some mild scrotal discomfort and swelling after the procedure, which typically subsides within a few days. Following the doctor’s advice on pain management and activity restrictions is crucial for a smooth recovery.
But don't they use a scalpel? Doesn't that part hurt?
In a conventional vasectomy, a scalpel is used to make small incisions in the scrotum. However, we only use the MSI no-scalpel vasectomy which uses specialised instruments to puncture the skin and access the vas deferens, reducing pain and recovery time.
How long until I'm really back at 100 percent after a vasectomy?
Most men can return to their regular activities within a week, but it’s essential to avoid heavy lifting or strenuous exercise for at least two weeks. It may take up to six weeks before you’re considered 100% recovered and your semen is sperm-free, which will be confirmed through a semen analysis.
How soon can I have sex after my vasectomy?
You can resume sexual intercourse and a total of 3 months before your semen is sperm free. However, it’s crucial to use another form of birth control until your semen has been confirmed sperm-free to prevent unintended pregnancies.
Can a vasectomy be reversed?
A vasectomy should be considered as a permanent form of male birth control, however, vasectomy reversal is possible, although not always successful and not always covered by insurance.